�¼������ϲʿ���ֱ�� the author: is the James Palmer Chair in Public Policy and Law and University Research Professor in the Schulich School of Law at �¼������ϲʿ���ֱ��.
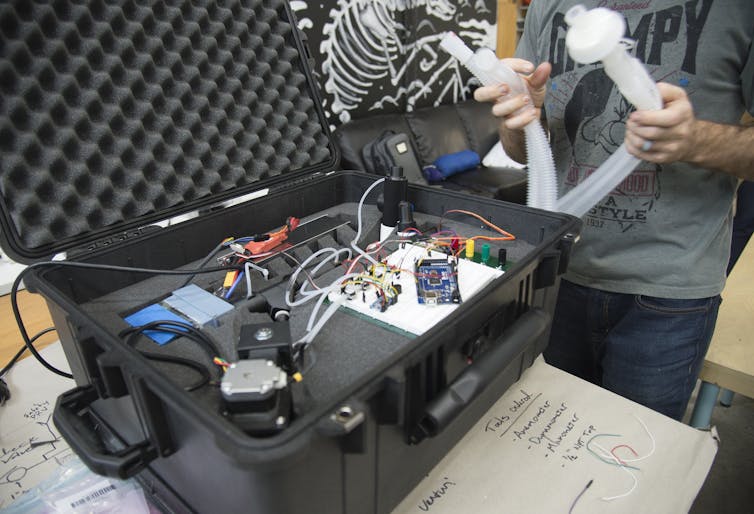
Across Canada, the coronavirus pandemic is increasing the demand for . In the coming weeks, there is a very real chance that there . Difficult decisions will have to be made about who gets what. Sick individuals who might survive if put on a ventilator may be denied access to one, or even removed from one they were already on, in order to save someone else.
In anticipation of this, : documents that spell out the nature and process of allocation decisions. The normal rules for allocating resources just . When critical care units can no longer admit everyone who wants and might benefit from critical care, new rules must be set. Who lives and who dies? Who decides?
Triage protocols vs. standards of care
The best case scenario is that these protocols will not need to be introduced, and it will be possible to meet all clinical needs through mobilization, management and sharing of resources. However, given the uncertainty about the future spread of the virus, we should hope for the best but prepare for the worst. Which means provincial and territorial governments should prepare critical care triage protocols, as .
However, for these protocols to work and not add more stress to our already over-stressed health-care providers, the authorities — including governments, prosecutorial services and professional regulatory bodies — must take steps to protect health-care providers. Authorities must ensure that health-care providers who follow these protocols will not face criminal or civil liability, or discipline by regulatory colleges, and ensure that health-care providers are aware of this.

The problem is that critical care triage protocols direct health-care providers to . They may direct providers to prioritize based on survival of the most people, or first-come-first-served or lottery. Furthermore, protocols may direct providers to discriminate based on grounds that are usually prohibited .
Liability risks
Normally, if a physician removes a ventilator from a patient who might survive, with neither the patient’s nor their substitute decision-maker’s consent, they might be charged with . The patient’s family might or claim a breach of . The province’s college of physicians and surgeons might discipline the physician for violating their .
However, a critical care triage protocol may direct a physician to do just that.
It’s possible that a court would not convict a health-care provider on criminal charges or find them civilly liable. It’s possible that a regulatory college would not find that a health-care provider breached professional standards.
On the other hand, it’s possible that there could be criminal charges, civil lawsuits and disciplinary hearings. It’s possible there could be liability and sanctions. Thus, these triage protocols can create both real and .
Protection and reassurance for providers
Fortunately, the authorities can protect providers from both liability and regulatory sanction, which can reassure providers. I will take Nova Scotia as an example; however, it is worth noting that the same or similar steps are available in other provinces and territories.
For criminal liability, the Nova Scotia director of public prosecutions could issue a directive indicating that criminal charges will not be prosecuted if health-care providers comply with the triage protocol and professional standards of their regulatory body. There are precedents for this; the and the have previously issued such directives about end-of-life care.
Furthermore, the federal government could publish a guidance document indicating its endorsement of a particular triage protocol or of triage protocols in general. While this would not have the force of law, it could be used in court should there be a need to defend against criminal charges laid against a practitioner for complying with their provincial or territorial triage protocol.
For civil liability, the minister of municipal affairs could approve a Nova Scotia critical care triage protocol as an emergency management plan under the . This would ensure, under the liability provisions of that act, that health-care providers are protected from any civil liability for actions taken that comply with the protocol.
For professional sanction, the regulatory bodies (such as colleges of physicians and surgeons) could issue stating that health-care providers must follow a triggered protocol and that health-care providers will not be subject to sanction if they do so.
If these steps are both taken and publicized by authorities and alike, health-care providers will be able to move forward without fear, safe in the knowledge that they are protected. This will allow health-care providers to follow triage protocols, which are established in accordance with the values and goals that society believes should guide the allocation of scarce resources during the present crisis.![]()
which features includes relevant and informed articles written by researchers and academics in their areas of expertise and edited by experienced journalists.
�¼������ϲʿ���ֱ�� is a founding partner of The Conversation Canada, an online media outlet providing independent, high-quality explanatory journalism. Originally established in Australia in 2011, it has had more than 85 commissioning editors and 30,000-plus academics register as contributors. A full list of articles written by �¼������ϲʿ���ֱ�� academics can be found on

