
Dr. Alyson Kelvin, vaccine research with the Canadian Center for Vaccinology and –¬º”∆¬¡˘∫œ≤ ø™Ω±÷±≤•‚Äôs Department of Pediatrics, sporting her protective hazardous materials suit.
Our world is changing — and research is changing with it. The Big Picture, a long-form Dal News series, provides an in-depth look at specific areas of research with global implications.
Between the coughing, sneezing, stuffy noses and watery eyes, it’s clear that we’re in the midst of cold and flu season, which serves as an annual reminder of the critical role vaccines play in the fight against the spread of infectious disease.
Thanks to immunization, which can be considered to be one of the most important advances in the history of public health, deadly infectious diseases such as measles, polio, and chickenpox are now all preventable.
Yet, the success of those same immunization programs — estimated to have saved more lives in Canada over the past 50 years than any other health initiative — has also helped spawn one of the most divisive health-care debates today: do we still need vaccines?
“Sometimes when we see success, it’s like an event,” says Dr. Joanne Langley, Division Head of Infectious Diseases, and a Professor in the Faculty of Medicine. “We’ve hit the goal, and that’s the end of it. But that’s not the case with infectious diseases.”
“Unless you eradicate the illness, infections are still out there and ready to come back, and the program of prevention should be continued. We know how to control diseases, but this is an effort that requires ongoing strong vaccination programs and for the public to be engaged and aware of the threat of disease if vaccination rates fall.”
Vaccines: A brief history
The practice of immunization dates back to ancient times, and coincides with the emergence of smallpox.
Smallpox is an ancient disease caused by a virus. There’s evidence that it affected the ancient Egyptians, with smallpox lesions being found on mummies. And techniques were developed in ancient China to try and stimulate the immune system, and make sure it was ready for the viral assault.
In the 18th century, English physician Dr. Edward Jenner noticed that women exposed to cowpox through their routine work milking cattle could be protected from the smallpox virus.
“Jenner stands out because he took that observation and started to perform experiments to show that if you were inoculated with cowpox, you can be protected from smallpox infection,” says Dr. Alyson Kelvin, a researcher at CCfV and an assistant professor in the Department of Pediatrics.
Another major milestone is the development of the influenza vaccine. Influenza has been around for thousands of years, but the cause for the illness was unknown ‚Äî¬Ýeven during the 1918 pandemic which killed an estimated 100 million people worldwide, it wasn‚Äôt known if people were dying from bacteria or some other pathogen.
In 1933, the virus responsible for what we now know as influenza-like symptoms, and shortly afterwards the first influenza vaccine was developed. Dr. Kelvin explains this coincided with the identification of a virus as an etiological agent and the cause of a major disease. During this time, researchers also figured out how to propagate the virus.
“If you don’t know what a virus is, or you don’t know where it comes from, and how it behaves, you can’t grow it and make a vaccine from it,” says Dr. Kelvin. “So the researchers who figured how to isolate influenza virus were then able to take it, grow it and make a vaccine.” These strategies were then used to develop the extremely successful polio vaccine, which has brought the poliovirus close to eradication, saving millions of lives.
–¬º”∆¬¡˘∫œ≤ ø™Ω±÷±≤• has its own notable spot in vaccine history. In 2014, a clinical trial for an experimental Ebola vaccine took place here, led by Dr. Scott Halperin, professor in Dal‚Äôs Division of Pediatric Infectious Diseases. Canadian researchers had already been studying a possible Ebola vaccine well before the pandemic occurred in West Africa, but their work was not overly visible. In response to the quickly escalating global crisis, the (PHAC) and the (CIHR) teamed up with the on a Phase 1 clinical trial of the VSV-ZEBOV vaccine on local residents. The results from this study were a key part of what led to the selection of the vaccine for a phase II-III trial.
The speed at which this vaccine was developed is considered extraordinary. Because emergency rapid response infrastructure was available, VSV-ZEBOV was available in just 12 months. Dubbed the ‚ÄúCanadian vaccine,‚Äù it is now a highly effective tool in the fight against the Ebola virus ‚Äî¬Ýa Canadian, and –¬º”∆¬¡˘∫œ≤ ø™Ω±÷±≤•, success story on the front lines of the battle against global illness.
From the bench to market
The typical vaccine can take about 10-15 years to get to market. It all starts in the lab, with an understanding of the disease along with its effects and how it is transmitted.
“A key part is understanding the immunity,” says Dr. Halperin. “That includes figuring out how someone becomes protected in the natural environment, what aspects of that organism causes disease, how the immune system responds to it, and determining if it is responding or protecting itself by making antibodies.”
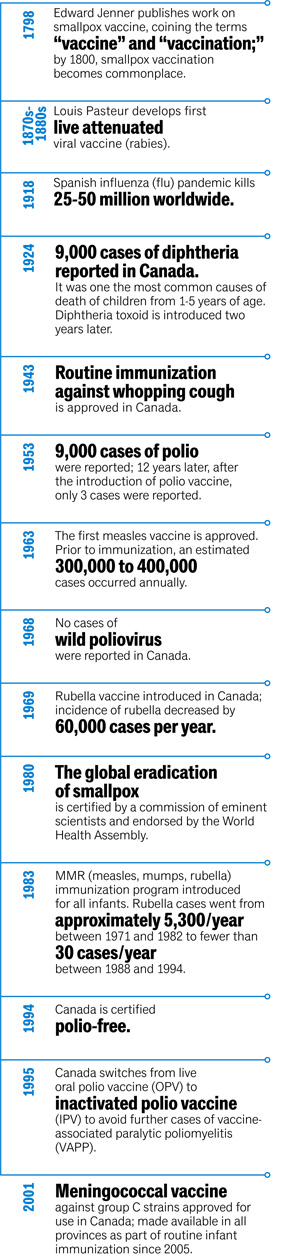
Source: Canadian Public Health Association
“What you want to do is give something that gives the same immune response to protect the person as it does after natural infection — but without getting sick. So it’s understanding that pathophysiology, and that’s all basic science research.”
Once the researchers identify how one becomes immune, the vaccine goes into development. There are all kinds of different strategies that can be used, including purifying a protein, attenuating a virus (weakening it) so it doesn’t cause disease, or making a viral-like particle.
“In the lab, researchers work to protect cell cultures from being infected by an organism, and then they look at it in multiple different animal models to test for safety,” says Dr. Halperin. “Then a phase one trial takes place, which is done with a very small group of people and with very careful monitoring.
 Dr. Scott Halperin, pictured in the IWK Health Centre.
Dr. Scott Halperin, pictured in the IWK Health Centre.
“If it passes the phase one study, then it goes into a phase two study, where one starts looking at it more towards the target population. In the phase three study, you’re looking at if it works. You immunize a group of people with the vaccine, another group with a placebo, and then you monitor them for development of disease over time.”
Dr. Halperin’s own research focuses on whooping cough, which is a respiratory infection. There has been a vaccine available for over 80 years, but there has been a resurgence of the disease in the past decade.
“We’ve been doing a lot of research to try and figure out why that is, how the vaccine can be improved, and how we can better use the vaccine,” says Dr. Halperin. “We had the idea to give the vaccine to pregnant women, which would help them develop antibodies that would be passed through the placenta to the infant. When it was implemented in the United Kingdom, it was shown to be 90 per cent effective in protecting infants in the first few months of life.”
As of last spring, this immunization program became the policy across Canada: it is now recommended that all pregnant women receive the vaccine.
“We don’t know what the uptake is yet, but some of the research we intend to do in the next year will look at that and try to see how well the program is being accepted,” says Dr. Halperin, who says it’s exciting that their work is now a publicly funded vaccine.
“We’ve been involved from the very basic design of the vaccine 20 years ago and have had the opportunity to see how it can be best be used in clinical trials, then being developed into policy. It’s run the whole spectrum of taking something from the bench to policy.”
Emerging virus research
Every now and then, a new virus emerges that causes illness, dominates the news cycle and sparks a rush to create a vaccine to protect people and prevent spreading.
It was in December 2019 that the first case of the Novel Coronavirus (COVID-19) was reported in China. It’s the third coronavirus to emerge in the past two decades (SARS in 2002, and MERS in 2012), and the health and economic impact it has had around the world has been significant.
According to an article co-written by Dr. Alyson Kelvin for The Conversation Canada, scientists from China were able to rapidly isolate the virus and sequence its genome using a cutting edge technology called next generation sequencing.
“ Next generation sequencing allows scientists to rapidly determine the genetic code of an organism,” says Dr. Kelvin. “It detects all variations or mutations in the genome, which may provide scientists with clues on mutation rates, the source of the virus and its pattern of circulation within a population.”
 Dr. Alyson Kelvin, at work in the lab.
Dr. Alyson Kelvin, at work in the lab.
A key part of Dr. Kelvin’s work is studying emerging viruses, like COVID-19, to determine what kind of disease they cause and develop specific vaccines to keep people from getting sick.
“The sequence of the viral genome also allows scientists to begin designing and synthesizing vital proteins for vaccine development. With the sequence available, a great number of researchers with a larger array of tools are able to work on vaccines and antivirals for this immediate viral threat.”
Although thousands have died of COVID-19 in little over two months, the Public Health Agency of Canada indicates that the overall health risk in Canada remains low. Due to the rapid spread of the virus and the number of deaths associated with infection, it is important to remain vigilant of Canadian and Provincial public health direction. There are currently no confirmed cases in Nova Scotia.
Still too much misinformation
According to Dr. Langley, parents think critically about health care and the value of interventions, but doctors often lack the time or resources to offer the kind of collaboration and consultation needed to ensure patients fully understand the benefits of vaccines.
“The public is very science literate, and answering their questions in a way that matches with their understanding and abilities is different in 2020 than it was in 2010,” says Dr. Langley. “We need to find ways to provide information that don’t rely completely on spending a lot of time with health-care professionals – because they don’t have that time.”
To fill gaps in their knowledge, some individuals turn to the internet or media for answers. ¬Ý
 Dr. Joanne Langley, division head of Infectious Diseases.
Dr. Joanne Langley, division head of Infectious Diseases.
While Dr. Langley agrees that it’s wise to have lots of good sources on social media, sometimes the tenor of discussion and the discourse on social media are not conducive to making good health choices.
“We know that there’s a lot of misinformation, dis-information and a lack of good information. So, how do we help people trust the sources of information, and find the good, accurate sources of information that are there?
“People often make decisions based on how they feel — and that’s invaluable. How do institutions become trustworthy? How does the health profession become trustworthy? There’s so many things we need to tackle, and we’re finding out more and more that if families have sources of information, and lots of chances to get their questions answered, they will decide to vaccinate.”
Vaccines from a social science perspective
For Dr. Janice Graham, an anthropologist in the Division of Pediatric Infectious Diseases, vaccines are more than medicine — they are social products.
“Vaccines are particularly interesting because they are developed for the public’s health, not simply individuals” says Dr. Graham. “This really appeals to the importance a society places on building a public foundation for universal health care, and I like to take a step back and look at the whole lifecycle production of vaccines. Who decides what vaccines for which populations, are they as safe and effective as they can be, and do all communities have equitable access to the vaccines they need? What is in the actual make-up of vaccines? What drives the need for, or hesitation in receiving, particular vaccines in particular populations?”
“The technical, political, economic and moral issues and decision-making are entangled, so I study them all together.”
Her three-year, CIHR-funded anthropological study generated and analyzed accounts of Ebola interventions from community members, health-care providers (formal and informal), biomedical researchers, government officials, NGOs and multilateral organizations. Her findings are being used to create a contextually sensitive and flexible decision-making framework to be used by national health authorities to prioritize health interventions and strengthen community health surveillance and response.
“We need better access to health care, strengthened health systems, well trained doctors and nurses, community workers and proper clinics with medication and supplies,” says Dr. Graham, who works in West Africa as well as Europe and Canada. “Low income countries often only get offered one-off programs that target a particular disease at a particular time, usually during an outbreak. In emergency situations, urgent response is absolutely necessary, but the outbreak might never have happened if adequate health care systems and medicines and vaccines were available from the start."
 Dr. Janice Graham, photographed in her office.
Dr. Janice Graham, photographed in her office.
In her opinion, a key part in handling these emergencies successfully is involving the people on the ground from the beginning. And, the Ebola crisis during 2014-2016 showed the importance of engaging with communities and working with anthropologists and other social scientists throughout epidemic response.
“Watching the sharing of local and international data and information that can take place to solve a problem, to resolve an epidemic, has been quite lovely,” says Dr. Graham. “Still, I would like to see more. I think we will, it’s moving that way. In the global health context, there’s an increasingly awareness of the importance of building capacity for qualified health personnel and infrastructures.
“I just wish that we were doing more towards training locals and securing sustainable health-care systems so that emergency responses would be fewer, and more quickly resolved. We’re making fantastic inroads in developing new vaccines for old and emerging diseases, but the ability to prevent outbreaks from happening in the first place, and responding effectively when they do occur, lies in the social determinants of health. Vaccines are one of the tools that are needed.”
Learn more about the world-class work being done by researchers like Dr. Halperin, Dr. Graham, Dr. Kelvin and Dr. Langley on the .
